Massachusetts’ healthcare system is under mounting pressure as burnout among nurses, physicians, and frontline staff fuels staffing shortages and strains patient care, according to hospital leaders and labor representatives. Years after the acute phase of the pandemic, clinicians cite longer shifts, heavier caseloads, administrative burdens, and rising workplace violence as key drivers, pushing more workers to leave or cut back hours.
The ripple effects are evident in longer emergency department wait times, closed beds, and increased reliance on temporary staff-trends that raise costs and risk access in both urban and rural communities. Policymakers, health systems, and unions are advancing competing fixes, from mental health supports and loan repayment to staffing standards, as the state confronts what many describe as a workforce crisis with no quick solutions.
Table of Contents
- Burnout strains Massachusetts healthcare workforce from Boston teaching hospitals to rural clinics
- Hidden drivers mount with staffing gaps mandatory overtime rising acuity and cumbersome electronic records
- Care access and safety erode as wait lists lengthen emergency department boarding persists and community hospitals face service cutbacks
- Blueprint for relief calls for enforceable staffing standards streamlined documentation expanded mental health supports flexible scheduling child care assistance and loan repayment to rebuild the pipeline
- Concluding Remarks
Burnout strains Massachusetts healthcare workforce from Boston teaching hospitals to rural clinics
From high-acuity academic centers in Boston to understaffed primary care outposts in the Berkshires, clinicians report escalating fatigue and attrition amid sustained demand and thin coverage. Hospital leaders cite double-digit vacancy rates, emergency department boarding that spills into hallways, and a steady drain of experienced nurses and physicians to travel contracts or non-clinical roles. Rural practices describe shrinking applicant pools and on-call burdens that stretch weeks, while safety-net facilities shoulder surges in behavioral health crises and delayed care. Front-line staff say the cumulative load-clinical complexity layered on administrative chores-has edged past sustainable limits. Key pressure points include:
- High patient volumes from respiratory illnesses, chronic disease backlogs, and rising behavioral health needs
- Persistent vacancies and overtime reliance that erodes morale and training time
- Administrative drag-EHR inboxes, prior authorization, and documentation mandates
- Workplace safety concerns, including verbal and physical aggression toward staff
- Cost-of-living strains that push clinicians farther from jobs or out of the field
Systemwide ripple effects are mounting: longer wait times for primary and specialty appointments, intermittent bed closures, maternity service cutbacks in smaller communities, and periodic ambulance diversions in urban hubs. Health systems are scrambling to stabilize operations with targeted incentives and redesigned workflows, even as unions press for enforceable staffing ratios. Measures under way:
- Retention bonuses, loan-repayment offers, and housing stipends to compete for scarce talent
- Team-based models that expand roles for NPs, PAs, and pharmacists, plus cross-training to flex coverage
- Flexible scheduling, protected recovery time, and on-site behavioral health services for staff
- Telehealth expansion and centralized scheduling to smooth demand across sites
- Policy moves under discussion, including scope-of-practice updates and streamlined prior authorization
Hidden drivers mount with staffing gaps mandatory overtime rising acuity and cumbersome electronic records
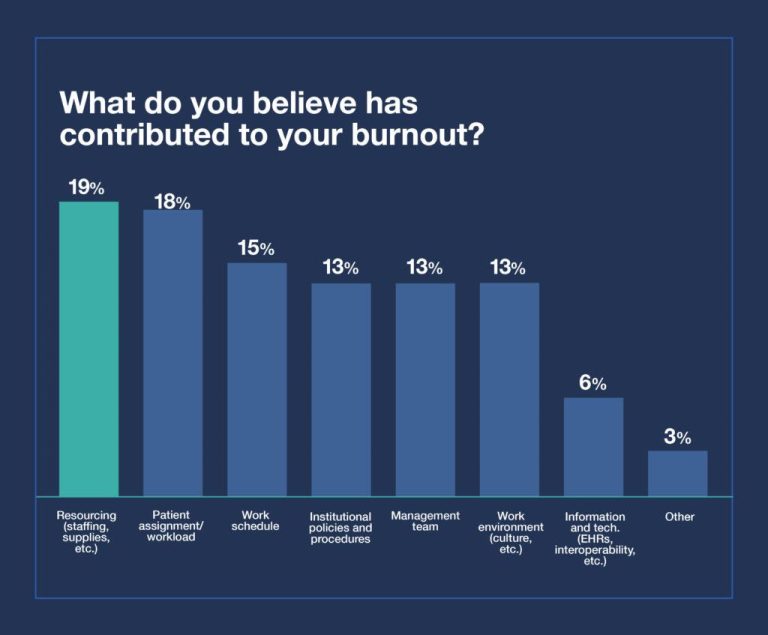
Across Massachusetts facilities, converging pressures are reshaping a normal shift into a marathon of interruptions and workarounds. Chronic understaffing forces clinicians to stretch across units, while higher patient complexity compresses already thin margins of time. Layered atop is an expanding digital burden: electronic systems that promise coordination but often deliver extra clicks, duplicate entries, and fragmented workflows. The cumulative effect is a steady rise in cognitive load and missed recovery windows between shifts-conditions closely linked to burnout and departures.
- Staffing gaps leave fewer hands for more tasks, widening care delays and inflating handoff risks.
- Mandatory overtime extends shifts beyond safe limits, eroding rest and decision-making quality.
- Rising acuity increases vigilance, escalation, and documentation needs per patient, straining ratios.
- Cumbersome EHRs pull clinicians from the bedside, adding clicks, alerts, and reconciliation steps that rarely align with real-time care.
The downstream impact is evident in schedule churn, reliance on temporary labor, and growing backlogs from emergency departments to community clinics. Leaders and frontline staff describe a system absorbing stress rather than solving it, with safety-net settings at particular risk. Stakeholders are pressing for targeted fixes that address daily friction points, not just headcounts, to stabilize teams and protect care quality.
- Flexible staffing pools and team-based models to cover surges without defaulting to forced overtime.
- Guardrails on consecutive hours and predictable scheduling to restore recovery time.
- EHR redesign-streamlined order sets, reduced duplicative documentation, scribes, and protected charting time.
- Retention incentives tied to precepting, specialty training, and high-acuity competencies that reflect actual workload.
Care access and safety erode as wait lists lengthen emergency department boarding persists and community hospitals face service cutbacks
Across Massachusetts, patients are encountering longer delays for appointments and procedures as workforce attrition constrains capacity. Emergency departments report prolonged boarding of medical and psychiatric patients, with stretchers occupying hallways and ambulance crews held out of service while waiting for handoffs. Clinicians describe a cycle in which burnout drives vacancies, vacancies drive backlogs, and backlogs elevate safety risks, including delayed diagnoses, treatment interruptions, and higher odds of adverse events in crowded settings.
- Primary care access: New-patient waits extend weeks to months, pushing more people to EDs for routine needs.
- Mental health bottlenecks: Scarce inpatient and step-down beds keep behavioral health patients boarding in EDs.
- Ambulance availability: Extended offload times contribute to ambulance diversions and slower response in some communities.
- Service reductions: Community hospitals scale back maternity, inpatient pediatrics, and elective surgical blocks to manage staffing gaps.
- Transfer delays: Tertiary centers receive more out-of-region referrals, but bed constraints prolong interfacility transfers.
- Equity concerns: Travel distances and costs rise for rural and Gateway City patients as local options shrink.
Financial strain, reliance on costly temporary staffing, and uncertainty around struggling systems have pushed smaller hospitals to consolidate services or pause programs, shifting volume to already burdened regional hubs. State-level steps-targeted workforce incentives, streamlined licensure, crisis coordination to reduce boarding, and oversight of at-risk facilities-aim to stabilize access, yet frontline leaders say the cumulative effects of staffing shortages and deferred care are still working through the system. The result is a fragile equilibrium: fewer local options, longer queues, and heightened pressure on clinical teams, with patient safety dependent on day-to-day surge management rather than durable capacity gains.
Blueprint for relief calls for enforceable staffing standards streamlined documentation expanded mental health supports flexible scheduling child care assistance and loan repayment to rebuild the pipeline
Under the proposal taking shape on Beacon Hill, state leaders and hospital executives are coalescing around a compliance-first framework that moves from recommendations to requirements. The plan would anchor care teams with binding staffing benchmarks, tighten oversight through real-time reporting, and trim low-value paperwork so clinicians can spend more time at the bedside. Health systems would receive technical support to standardize charting and reduce duplicative inputs, while regulators phase in accountability measures tied to quality and safety outcomes.
- Enforceable staffing standards: Graduated ratios by unit acuity, transparency dashboards, and escalating penalties for chronic noncompliance.
- Streamlined documentation: Unified EHR templates, elimination of redundant fields, and targeted relief from nonclinical administrative tasks.
- Data and oversight: Public reporting of vacancy, turnover, and overtime; independent audits to verify on-the-floor staffing.
- Workflow modernization: Scribe support, bedside charting pilots, and interoperability milestones to reduce re-entry of data.
The second plank invests directly in the workforce to blunt burnout and rebuild the pipeline. The package prioritizes confidential mental health services, expands flexible scheduling to stabilize coverage without overreliance on overtime, and lowers barriers that push clinicians out of the field. Advocates say targeted incentives-paired with faster licensure pathways-could restore capacity ahead of winter surges and stabilize hard-hit safety-net providers.
- Mental health supports: 24/7 peer lines, protected time for counseling, and insurance coverage without career repercussions.
- Flexible scheduling: Self-scheduling, shift-swaps, and float pools with premium differentials to ease bottlenecks.
- Child care assistance: Onsite centers, extended hours, and subsidies for overnight and weekend coverage.
- Loan repayment and training: Expanded repayment for high-need roles, paid residencies and apprenticeships, and expedited recognition of internationally trained clinicians.
- Accountability: Quarterly targets for retention, patient throughput, and agency reliance, with funding tied to measurable improvement.
Concluding Remarks
For now, the forces driving burnout in Massachusetts’ hospitals and clinics show little sign of easing, even as administrators expand wellness programs and lawmakers weigh broader workforce fixes. Nurses’ unions, physician groups and patient advocates agree on the stakes but diverge on timelines and tactics, underscoring how difficult it will be to stabilize staffing while demand for care remains high.
With the respiratory season ahead and budgets tightening, health systems face immediate pressures alongside longer-term questions about training pipelines, retention incentives and safe staffing. State officials say additional steps are under consideration. Whether those measures can arrive quickly enough to blunt further attrition-and protect patient access-will be a key test in the months to come.