Smaller community hospitals are entering a new financial reality. Pandemic-era aid has faded, labor and drug costs remain elevated, and more care is shifting to outpatient settings where payment rates are lower and margins thinner. At the same time, insurers are tightening authorizations and denials, while higher interest rates make it more expensive to maintain facilities and invest in technology. The arithmetic is unforgiving: costs are up, revenue growth is uneven, and cash reserves are under pressure.
The stakes reach beyond balance sheets. In many towns, the community hospital is the first – and only – point of access for emergency care, obstetrics, and behavioral health. When units close or hospitals downsize, ambulance rides get longer, outcomes can worsen, and local economies lose one of their largest employers. Even where doors stay open, service-line cuts and staffing shortages are reshaping what care is available close to home.
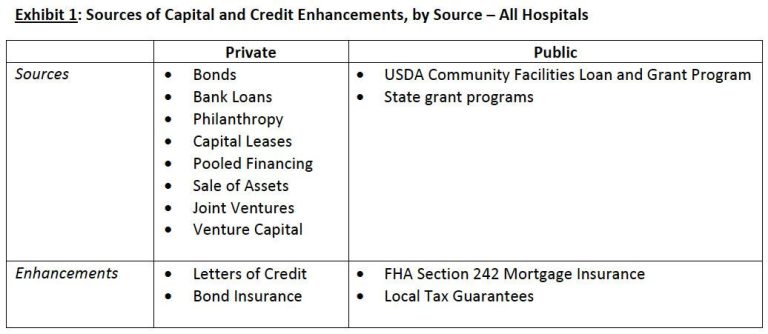
This article examines the forces squeezing smaller providers and the strategies they are using to stay solvent: tighter revenue-cycle management, payer negotiations, selective service consolidation, partnerships or mergers, and new federal options such as the Rural Emergency Hospital designation. It also explores the policy choices that could change the trajectory – from Medicaid expansion and global budgeting experiments to targeted grants and workforce pipelines – and the metrics that matter, including operating margins, days cash on hand, debt loads, and capital needs.
Table of Contents
- Medicaid Mix and Low Commercial Rates Erode Operating Margins in Critical Access Facilities
- Strategic Partnerships and Shared Services Cut Overhead Without Sacrificing Local Control
- Investing in Outpatient Behavioral Health and Infusion Lines Stabilizes Volume and Revenue
- Data Driven Revenue Cycle Cleanup and Denials Management Deliver Immediate Cash Improvements
- Concluding Remarks
Medicaid Mix and Low Commercial Rates Erode Operating Margins in Critical Access Facilities
Operating margins at rural hospitals are being pinched as a heavier payer mix skews toward Medicaid while commercial contracts remain thin. Administrators report that reimbursement floors are failing to keep pace with inflationary cost growth, and outmigration to larger systems is diluting higher-yield procedures. With limited leverage in concentrated insurance markets and escalating wage, drug, and purchased-service expenses, leaders say the traditional cross-subsidy from commercial payers is narrowing, exposing small facilities to volatility in volume and case mix.
- Reimbursement pressure: Medicaid base rates and add-ons lag rising acuity and input costs; commercial allowables remain conservative in narrow-network geographies.
- Volume shifts: Outpatient migration and referral leakage to tertiary centers erode contribution margins on key services.
- Cost inflation: Contract labor, pharmacy, and supply chain volatility outstrip rate updates.
- Capital constraints: Limited reserves and higher borrowing costs compress flexibility for service upgrades and staffing stabilization.
In response, executives are pursuing targeted moves to stabilize cash flow while maintaining access. Contracting teams are pressing for rate floors, outlier protections, and drug carve-outs, while finance leaders intensify capture of DSH/UPL, directed payments, and 340B savings. Systems are also realigning service portfolios and deepening affiliations to protect essential care and smooth referral pathways, with technology and workforce redesigns used to control unit costs.
- Payer strategy: Leverage price-transparency data to benchmark commercial rates; prioritize escalators and carve-outs for high-cost episodes.
- Supplemental funding: Optimize Medicaid supplemental programs and documentation; tighten cost reporting to reflect true acuity and expenses.
- Service configuration: Consolidate low-volume lines, expand telehealth and virtual specialty coverage, and optimize swing-bed utilization.
- Workforce and revenue cycle: Reduce agency reliance via internal pools and cross-training; strengthen eligibility screening, pre-authorization, and denials management.
Strategic Partnerships and Shared Services Cut Overhead Without Sacrificing Local Control
Hospital executives facing inflation, workforce shortages, and payer pressure are increasingly turning to alliances that pool nonclinical functions while keeping community decision-making intact. Leaders describe a shift from full mergers to targeted collaborations that deliver scale where it matters-procurement, back-office, and technology-without diluting local identity or clinical priorities. Early adopters report streamlined operations and improved negotiating power with vendors, as standardized playbooks and shared infrastructure replace duplicative overhead.
- Group purchasing and standardization: Regional buying councils negotiate lower prices and align formularies and supplies across facilities.
- Shared back-office hubs: Centralized revenue cycle, HR/payroll, and pharmacy management reduce administrative burden and speed cash flow.
- Clinical resource sharing: Co-managed service lines and flexible staffing pools support coverage for imaging, anesthesia, and specialty call.
- Technology cooperatives: Joint EHR optimization, cybersecurity services, and telehealth platforms cut IT spend and improve uptime.
Industry analysts note that the most durable models are built on explicit guardrails: local boards retain authority over service mix, physician alignment, and community benefit, while shared services operate under measurable performance terms. Contracts are increasingly structured to be modular and time-bound, so hospitals can scale participation up or down as conditions change-capturing savings without locking into inflexible structures.
- Local governance preserved: Community boards set strategy and keep final say on clinical programs and capital priorities.
- Menu-based participation: Hospitals opt into specific functions-such as supply chain or IT-rather than wholesale consolidation.
- Transparent cost allocation: Activity-based pricing and quarterly scorecards tie fees to measurable outcomes.
- Data and privacy safeguards: Shared analytics with role-based access maintain compliance and trust.
- Sunset and exit options: Periodic reviews and off-ramps protect flexibility if goals or market dynamics shift.
Investing in Outpatient Behavioral Health and Infusion Lines Stabilizes Volume and Revenue
Community hospitals are turning to outpatient behavioral health clinics and hospital-based infusion suites to smooth demand and protect margins amid shifting inpatient case mix. Leaders describe these service lines as reliable access points that convert unpredictable admissions into predictable, scheduled volumes, curb ED boarding for psychiatric crises, and retain complex therapy patients locally rather than losing them to regional centers. Infusion capacity tied to oncology, neurology, and rheumatology also anchors specialty pharmacy relationships, while coordinated behavioral health follow-up reduces readmissions and supports value-based contracts by addressing high-cost, high-need populations.
- Volume smoothing: Appointment-driven throughput balances seasonal inpatient swings and optimizes staffing.
- Revenue durability: Buy-and-bill infusion therapies and steady behavioral health visits diversify the payer mix and reduce outmigration.
- Access and equity: Same-day telepsychiatry, intensive outpatient programs, and local infusion reduce travel and wait times.
- Operational relief: Fewer avoidable admissions and shorter ED holds free beds for higher-acuity cases.
Administrators emphasize that execution determines returns: right-sized footprints, integrated referral pathways, and pharmacy-readiness are critical, as are partnerships with psychiatrists, advanced practice providers, and licensed therapists. Observers note that aligning site-of-care strategies with payers, investing in care navigation, and standardizing protocols for biologics can protect gross-to-net while improving patient experience and clinician workflow.
- Demand and network mapping: Quantify local need, leakage patterns, and primary/specialty referral sources.
- Payer alignment: Contract for site-of-care shifts, tele-behavioral parity, and infusion coverage policies.
- Care model and staffing: IOP/PHP design, collaborative care in primary care, and cross-trained infusion RNs.
- Pharmacy and compliance: Buy-and-bill governance, sterile compounding standards, and prior auth workflows.
- Navigation and retention: Closed-loop referrals, social work support, and post-discharge follow-up to minimize leakage.
- Outcomes tracking: ED boarding hours, no-show rates, therapy completion, and total cost of care benchmarks.
Data Driven Revenue Cycle Cleanup and Denials Management Deliver Immediate Cash Improvements
Smaller community hospitals are tapping analytics to tune up the revenue cycle and pull cash forward, even amid staffing shortages and payer friction. By consolidating registration, coding, charge capture, and contract data into a single view, leaders are surfacing the biggest leaks-aged A/R, small-balance write‑offs, avoidable late charges, and underpayments-and fixing them at the source. The operational shift is pragmatic: normalize payer rules, harden front‑end edits, reconcile charges daily, and align work queues to the highest return. Early outcomes reported by finance teams include:
- Higher clean-claim rates through pre-bill edits and eligibility verification
- Faster cash acceleration via daily charge reconciliation and DNFB reduction
- Lower avoidable write-offs as small-balance workflows and timely filing safeguards tighten
- Contract compliance gains using automated underpayment detection and payer variance monitoring
Focused denials control is the parallel lever, with root-cause analytics, automation, and payer-specific playbooks converting blocked revenue without adding headcount. The approach is preventative first, then recovery at speed: trend denial codes by service line and site, push fixes upstream, and industrialize appeals where overturn rates are highest. Hospitals prioritizing this model are standardizing the following:
- Real-time eligibility and authorization checks with proactive rescheduling rules
- First-pass coding accuracy supported by CDI prompts and medical necessity checks
- Automated attachments and clinical packets tailored to payer templates
- Appeals kits and scripting triggered by denial propensity and timely filing clocks
- Payer scorecards and executive escalations tied to contract terms and response SLAs
Concluding Remarks
For smaller community hospitals, the financial picture remains fragile: expense growth continues to outpace revenue gains, margins are thin, and access to capital is limited. Temporary boosts-from pandemic-era relief to short-term rate adjustments-have faded, leaving administrators to balance rising labor, drug, and supply costs against fixed payments and unfavorable payer mixes.
To stay viable, many are narrowing service lines, shifting care to outpatient settings, and pursuing affiliations that promise scale without sacrificing local control. Telehealth, hospital-at-home programs, and joint purchasing agreements are emerging as stopgaps, while targeted designations and supplemental payments offer lifelines in some states. Yet each option carries trade-offs in autonomy, access, and long-term resilience.
What to watch next: state decisions on Medicaid expansion, uptake of Rural Emergency Hospital conversions, scrutiny of 340B savings, and the trajectory of labor markets and interest rates. Bond downgrades, rising bad debt, and utilization shifts will signal whether incremental fixes can hold-or whether more consolidation and closures follow. For the communities that depend on these hospitals, the stakes are immediate: maintaining timely, local access to care as the economics grow harder to ignore.